Maternity crisis deepens as Q'town hospital goes unstaffed

The maternity ward at the Lakes District Hospital was unstaffed overnight this weekend as the district deals with a worsening shortage of midwives.
Janeen Holmes, the operations manager at the hospital, told Crux staff illness and leave had left them unable to fill their roster.

Janeen Holmes - no SDHB midwives to provide cover this weekend
The maternity ward remained open for births, but a Lead Maternity Carer (LMC) midwife had to have their back-up midwife in tow for a birth during the overnight shifts.
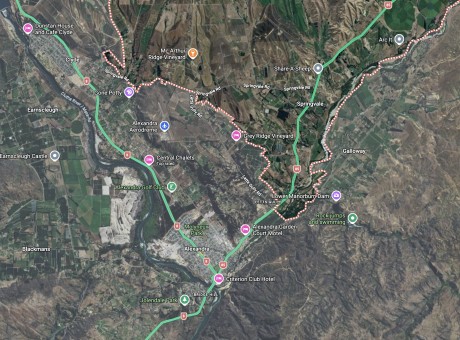
It comes on the heels of a similar curtailing of services at Alexandra’s Charlotte Jean maternity hospital.
In July Charlotte Jean was left unmanned on two occasions as they battled staff illness and roster gaps.
As was the case this weekend in Queenstown, Charlotte Jean management told local LMC midwives the hospital could only be used for births during those times if a second midwife was provided for back-up.
In addition, new mums and their babies wanting to stay at Charlotte Jean for post-natal care after birthing in the big smoke were unable to be admitted.

Waitaki MP Jacqui Dean - the region is dealing with a chronic shortage of midwives, and the situation is worsening.
Waitaki MP Jacqui Dean says the region is dealing with a chronic shortage of midwives, and the situation is worsening.
Queenstown midwife Keri Mapperson agrees. She’s not afraid to call it a crisis. But she says it’s nothing new.
It’s always going to be tougher for midwives working in the regions and rural settings, she says.
“It’s not like it’s a city, with a huge pool of spare staff.”
Plus, there’s the added professional stresses that come from always being removed from a higher-level base hospital.
She’s keenly aware, for example, when she steps outside on days when the weather is rough, of whether a helicopter will be able to take-off or roads might be icy or impassable with snow.

Queenstown midwife Keri Mapperson - "The population is pushing the limits of what’s sustainable."
Add on the rapidly rising cost of living in the region and it’s not hard to see why retaining midwives is a challenge, she says.
For Keri, it’s also an issue of equity. The region is screaming for a level two hospital. Blenheim and Gisborne, comparable locations yet without the projections of population growth or the isolation factors, have them.
Doctors, nurses and midwives are “working their butts off” to provide an “incredible service”, she says.
“But they’re working on the edge of what’s OK. The population is pushing the limits of what’s sustainable.”
Central Otago midwife Charlotte Aarden works in miracles.
On a daily basis, in her line of work, she gets to be a part of one of life’s most precious events.
Childbirth, she says, is beautiful. Less so, the increasing challenges of working as an LMC midwife in the region.
She’s worked for more than 11 years in Central Otago and, despite population growth, she hasn’t seen much change in services in that time.
It contributes to a shortage of midwives, she says.
“It is simply not attractive to work in such a challenging environment.
“I’m kind of used to a midwife crisis.”
She’s been forced to think about how she practises and, in turn, that affects the experience of her clients.
The safety of mums and babies comes first, and often pro-active decisions are made to deliver in a hospital setting, she says.
“So that you don’t end up in a situation where an ambulance or chopper isn’t available when you need it, or be separated from your (the mother’s) partner.”
And there’s financial implications that come with that for a midwife. She earns less for a hospital birth, there may be hotel costs, and there’s always long hours, time away from her own two children and a potentially dangerous amount of travel.

Midwife Charlotte Aarden - If she had a magic wand, she’d be with her Queenstown colleague Keri Mapperson, magicking up a hospital for the district.
“My biggest fear is not to be able to come home to my family due to an accident…Having two children and one on the way, this is really scary. Nobody helps you to be safe…There is no health and safety for midwives as there is for ambulance staff, truck drivers or doctors, for example.”
The Southern District Health Board has stepped up, providing LMC midwives in its catchment with a $300 top-up per client in addition to what they receive from the Ministry of Health.
It’s welcome, of course, but for Charlotte it’s still money well-earned.
In a city set-up, the responsibility of a difficult birth is transferred to a team led by an obstetrician. In this neck of the woods, there may be ambulance or chopper transfers involving high-risk care that lands on the shoulders of the midwife. And, in these cases, she receives the same funding from the Ministry of Health as for a standard primary care birth, she says.
“So, the extra risk and complications, travel, time and costs are not recognised.”
If she had a magic wand, she’d be with her Queenstown colleague Keri, magicking up a hospital for the district.
“What they do in Blenheim would be magic in this region. Similar population and a small hospital that is covered by a rotation of obstetricians, paediatricians, and anaesthetists from Nelson and Christchurch.
“I think we need such facility here and a rotation between Invercargill and Dunedin.”
Heading into the weekend, Charlotte says she had two women “on the niggle”, so she’d checked in with Charlotte Jean to ask about potential roster issues.
There were none.
Sue and Roger O’Brien, who manage the privately-owned Charlotte Jean maternity hospital in Alexandra, have told Crux they feel confident with their staffing stability.
They’re contracted by the Southern District Health Board (SDHB) to provide primary birthing services for the district, and in the past 10 months, through negotiations, have secured a 13 percent increase in their annual contract value. Although, the final increase installment hasn’t quite hit their books yet.
It means they can pay their own midwives more – an important equity issue as DHB-employed midwives this year benefited from a successful collective pay agreement that left midwives employed by the likes of Charlotte Jean a step behind.

The privately owned Charlotte Jean maternity facility in Alexandra - heading for a record year.
They are also tapping into a pool of locum midwives; a fact MP Jacqui Dean is heralding as evidence the system is failing.
But Roger O'Brien is pragmatic, saying it’s a reality in rural healthcare, and it’s worked successfully for them.
 He does agree with Jacqui, however, that there is a midwifery crisis. But the region is certainly not the only one faced with such challenges – the issues are nationwide, he says.
He does agree with Jacqui, however, that there is a midwifery crisis. But the region is certainly not the only one faced with such challenges – the issues are nationwide, he says.
“There’s been some temporary fixes, but they don’t address the lack of a sustainable workforce, the wider issue.
“It’s time that there is a re-examination of the whole system.
“Midwives do an amazing job of looking after mums and babies. People need to start looking after midwives.
“If the issues are not addressed there will be risks.”
Last year, Charlotte Jean recorded its highest number of women admitted. This year to date, births are already at 75 percent of 2018’s total.
Roger says he has concerns any future health planning may be affected by outdated population data. Keri, in Queenstown, feels the same.
The 2018 Census has been something of a headache for statisticians, so bodies like DHBs are forced to work with stale data. In a region of growth like Central Otago and the Lakes District, the data is staler than most.

Health Minister David Clark - does the buck stop in Wellington as DHB's are forced further into the red?
The issues are complex, Roger says. However, for him and wife Sue, the job is simple: to do what’s best for whanau in their care.
“It’s about trying to manage it the best way we can. There’s a lot happening around, but that’s our focus.”
And they want women across the region to feel assured by that.
“It’s hard when you get these words of crisis thrown about…we worry about what the women feel.
“At the end of the day, everyone is working hard to make it work.”
The politics of birth for women in Central Otago and the Lakes District
The experience a Kiwi woman has while pregnant, giving birth and in the first weeks with a newborn is very dependent on where she lives because the power to fund facilities and services lies in the hands of the DHB – for us, that’s the Southern District Health Board (SDHB).
A woman generally chooses a Lead Maternity Carer (LMC) early on in pregnancy – it could be a GP or an obstetrician but in the vast majority of cases (94 percent in 2018) it’s a midwife.
Most LMC midwives are self-employed and paid by the Ministry of Health.
In Central Otago and the Lakes District, LMC midwives can access both the Charlotte Jean maternity hospital in Alexandra and the Lakes District Hospital in Queenstown any time and provide care from these facilities, supported by the core midwives and nurses who are employed there.
In Queenstown, the core midwives are employed by the SDHB, while in Alexandra, Charlotte Jean is the employer.
Both these facilities are primary birthing units. LMC midwives might also deliver babies at Dunedin or Southland Hospitals, especially in more complicated cases.

The SDHB's CEO Chris Fleming - the target of "frustration and disappointment" from Health Minister David Clark.
At the time of publishing, the SDHB had not responded to question from Crux, other than to confirm the gaps in the roster at the Lakes District Hospital over the weekend.
We do know there are two separate independent reviews underway relating to maternity services in the SDHB. One is something of a report card on the implementation of a new system of maternity care finalised by the SDHB in 2018 – a strategy called “Creating an Integrated Primary Maternity System of Care Across the Southern District”.
It resulted in Lumsden Maternity Centre being downgraded from a primary birthing unit to a maternal and child hub - a non-birthing unit (except in urgent situations) focusing on supporting antenatal and postnatal care. Wanaka also made the list for such a hub.
The Ministry of Health did reply to question from Crux, saying it was aware the SDHB and local maternity facility providers had been struggling to fill some rosters.
The ministry’s Clare Perry says she is confident systems are in place to ensure women receive the care they need, as ongoing efforts continue to improve staffing and provide back-up midwifery support.
In the last month, Ministry officials have participated in meetings with representatives from the SDHB, local midwives, GPs, and the NZ College of Midwives, among other stake holders. Progress is being made and they will continue working together to find solutions that work for the local communities down south, she says.
Budget 2019 contained some significant wins for midwives, including close to $7.5 million per year to allow a pay rise for LMCs and other maternity carers. That’s an increase of almost five percent, on top of an almost nine percent increase the previous year.
New funding to the tune of $4.5 million was also tagged for overall rural and regional workforce training and development, including a boost for locum support for rural midwives.