'I'm sick of waiting'. Inadequate facilities frustrating, unsafe for Wānaka midwife

Justine Quirke, a Central Lakes midwife of 20 years is asking, what's the hold up with Wānaka’s Primary Birthing Unit, and when will Central Lakes women have safe maternity care?
“A lot of those women may not have chosen to birth locally or may not be well enough to be recommended to home birth… but they haven’t the option to go to a hospital, because the promised birthing unit is not open.”
At the moment, local midwives are left in "risky" situations, trying to provide labour and birth care.
"You could do the best job in the world but you're still at risk of having a mum or a baby die, because you can't get them to the hospital where they're meant to be birthing," Ms Quirke says.
"They're either closed, short-staffed, or there's no transport available."
Behind Ms Quirke is the building purchased by Health New Zealand at ab estimated value of $2million to serve as Wānaka’s primary birthing unit.
Well past of the scheduled opening date of early 2023, it’s still a construction site. Midwives have been recently told that unit will not be ready until the end of 2024.
"I am sick of waiting for our promised birthing unit."
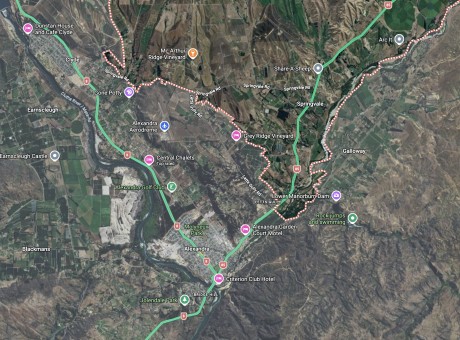
Working as locum in the area, Ms Quirke says she often has home births, because they are so far from maternity care, particularly Wānaka women, who are over an hour from primary birthing care.
Despite her love of midwifery, Ms Qurike herself is cutting back her hours, telling Crux, “It’s a numbers game”.
“I know there have been situations where babies have died. Although I personally haven't had that experience myself, I am now doing very little because it is a numbers game’.
She puts some of the experiences she has down to luck, working in a pressured, and short-staffed system, with an increasing number of patients.
And Central Lakes is an area with unpredictable weather, and the journey to the two closest base hospitals involves crossing mountainous road, frequently snowy and icey.
“I remember in the past being stuck at the Alexandra birthing unit all night with a woman who never should have been birthing in a primary unit. She was very high risk, had had a previous caesarean section but because it was snowing, we couldn’t get a helicopter, and we couldn’t get an ambulance.”
"It was a very isolating feeling."
She’s has also waited up to six hours for a helicopter transfer with a woman in an unstable condition, and says the experience was “really stressful for the family”.
The number of people birthing in the area is "growing and growing" every year, she says.
In the past 12 months ending October 2023, the Queenstown Lakes District grew by 8 per cent in data released by Stats New Zealand.
It's the biggest growth of any district in New Zealand, the data showed nationally, the country's entire population had a 2.1 percent growth.
Queenstown Lakes District Council estimates 52,020 people live within the district.
The district includes Wānaka, which is just over an hour’s drive away from the Alexandra birthing unit or the Queenstown’s Lakes District Hospital, which both only offer primary care – so no epidural, no cesarean section are available if needed.
Tertiary maternity care is over three hours drive away at Dunedin Hospital.
Every day, or at least “every other day”, Ms Qurike says a Central Lakes woman in labour is transported to Invercargill or Dunedin Hospital to receive a higher level of care during the birthing process.
“A lot of midwives are leaving the profession, because when they do work, they're put under so much pressure, that they can't provide good care. The NZ College of Midwives and locum service are a great support in fighting for better pay and conditions for midwives.
“However, it’s just too much stress.”
Turnover is high, but she believes if the facilities were up to scratch, there wouldn’t be an issue attracting more midwives to the region.
It’s a great place to live, she says.
On Christmas Day 2023, the Dunedin Hospital had more mothers from Queenstown Lakes, than those from did Dunedin.
And over the Christmas period, the short-staffed Invercargill hospital had put a “divert” on for four days, meaning they were not taking transfers from the Lakes District Hospital – which Crux has been told is a common occurrence.
And due to the two general practitioners in Wānaka closing at 6pm, the local ambulances are far more busy, making it take longer for birthing mothers to receive transport.
“There’s just so much pressure on the system,” Ms Quirke says.
Since the current system is to airlift away anyone in critical condition, Ms Quirke says this creates extra dangers.
“What happens when you travel by helicopter, is the mum has to fly on her own, and the partner then has to travel by private car. If the baby has already been born and there are health risks with the mum, she goes in the helicopter, and the baby then has to travel in the back of a car with the partner driving – who has often been up for two days without sleep.”
“That in itself is very dangerous.”
Ms Quirke says every week a sleep-deprived partner will drive through the gorge to Dunedin Hospital with a new born baby, in total, a four-hour trip.
Queenstown-based midwife Keri Mapperson tells Crux that on three occasions in the past two years, women have travelled two hours to birth in Invercargill, returned home, only to be helicoptered back to the hospital within the first eight days of the baby’s life.
She says these three cases were due to the baby’s having respiratory, cardiac and infection problems post-birth.
Ms Mapperson says there would “definitely be more” instances of this happening with other Queenstown midwives.
However, maternity is the “tip of the iceberg”, another Southern-based public health employee has said to Crux this week.
This employee can only comment in an anonymous capacity.
When a Queenstown woman goes into labour, "they have to decide whether or not they want to drive a long distance", the employee says.
"They either have to make the decision to travel in early labour, or birth in Queenstown [at the Lakes District Hospital] and have the potential for transfer... if they have risk-factors, they have to travel."
“Nobody should have to do that, they should be able to birth in their community.”
But maternity transfers, although frequent, are a very small percentage of the total transfers out of Lakes District Hospital, the employee says.
Lakes Hospital's rural emergency department only offers assessment and stabilisation, there are no surgeons, no operating theatres.
Patients with serious strokes, heart attacks or seizures are transferred to Invercargill or Dunedin Hospital, as well as those with broken bones, or those with mountain biking or skiing accident.
There's also only ten beds in the emergency department.
As a result, the employee is concerned with the way Queenstown is advertised internationally and domestically.
“Tourists think this is a place to come and do adventure sports, but it’s not… it’s not a world class resort.
“If people come here, they are at the mercy of a massively underfunded medical facility.
"If they fall off their mountain bike and waste their neck, they’re going to be put in a helicopter, or they’re going to be put in an ambulance to Invercargill and wait three days for surgery.”
“They [tourists] should be able to think that they’re coming to somewhere safe, that they won’t be flown to another city that’s hours away.”
The employee thinks that tourism companies should be helping the community lobby for a better hospital facility, but doesn’t think it’s something they’d be happy to open a dialogue about.
“It has to affect where the money is being spent, it has to affect tourism… tourism bosses will not want to admit that this is not actually a world-class resort.”
Southland's recently re-elected member of parliament Joseph Mooney says in the long term he believes that the Central-Lakes region will need more localised health services given the population growth and visitor numbers.
"Queenstown-Lakes had the biggest increase in population in the country last year, following average growth of 6.8% between 2013 and 2018, and with that comes a number of infrastructure challenges including healthcare."
He's been asked by Crux how he plans to advocate for and improve Queenstown and Southern's healthcare in his three year term.
In his written response, Mr Mooney says he has had and continue to have discussions with his colleagues and others about the healthcare needs of Queenstown-Lakes, Central Otago and Southern.
"I will continue looking into what further options may be feasible for our region, while being realistic about the challenging books that the new government has inherited."
Mr Mooney says that new Health Minister Shane Reti has committed to the rebuild of Dunedin hospital including reinstating all of the beds that the previous government removed and says this will help.
He says he will also be strongly supporting Minister Reti in boosting frontline numbers - one of the minister's main priorities for improving healthcare in regional New Zealand
And Mr Mooney acknowledges "the excellent work that our local healthcare staff do".
Crux has also spoke with the health minister, a former trauma surgeon, a West Coast mayor and Queenstown resident with two auto-immune diseases about the state of Lakes District's healthcare.
Read the piece here: Doctor: 'What's the point of the Lakes District Hospital?'