Doctor: 'What's the point of the Lakes District Hospital?'

What's the point of the Lakes District Hospital? A rhetorical question a Tasman-based doctor asked Queenstown patient Casey Todd last week.
As a local resident with two auto-immune diseases, Ms Todd asks herself the same question.
"He said to me, what's the point of it because it's got bugger all rooms. It's got basically no maternity ward, there's only four or five beds there, and the A&E department, they just lift everyone off to Invercargill or Dunedin."
She'd travelled down to Invercargill for this rheumatology appointment, one of six out of district trips to access healthcare for herself and her mother for 2023, fronting the cost themselves. They're not the only ones.
Many mothers will travel to Invercargil or Dunedin when they enter labour, rather than risking it at Lakes Hospital where there will be no epidural or emergency c-section available.
Also no surgical ward, no critical care unit, and only ten beds in the emergency department - anyone in a serious condition will be choppered to Dunedin or Invercargill due to the limited 'assessment and stabilisation' level of care provided locally.
Significantly underserved
Comparing Lakes District to other populations in New Zealand, Queenstown Lakes and Central Otago are significantly underserved.
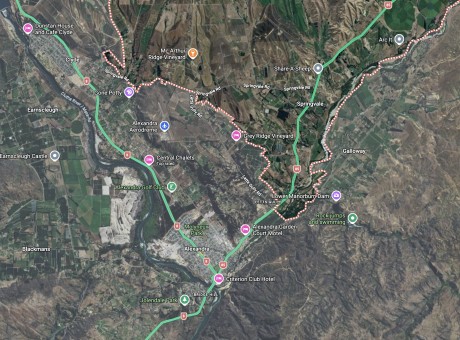
The hospital serves the Queenstown Lakes, which according to Queenstown Lakes District Council estimates is 52,020 people in 2023, a number that jumps to 63,640 in ten years, and 74,450 in 2043, but it also sees patients from Central Otago towns of Cromwell, Alexandra, and Roxburgh.
Plus more than a million tourists annually.
It's got 25 beds, and its closest base hospital is a two-and-a-half-hour, 183-kilometre drive away via the Devil's Staircase - Southland Hospital.
Comparatively, Marlborough District has Wairau Hospital in Blenheim, with 65 beds, and the larger Nelson Hospital is only one hour 44 minutes, or 118 kilometres, away by car. The Marlborough District population is 37,790.
There's also Timaru Hospital, which has 135 beds with secondary maternity, mental health, oncology, and surgical services, and a dementia ward. It services the South Cantebury area, populated by 52,785, according to the former district health board.
Queenstown and Wānaka's population boom and its impact on health infastructure was outlined in 2011 by the Association of Salaried Medical Specialists in a report titled 'New Public Hospital for Queenstown 2026'.
The warped facilities to population ratio in this area was pointed out, as was the need for a new hospital by 2026.
"Up until now, it is probably fair to say that most residents have accepted that, by and large, a two-hour-plus drive to the base hospital is the price you pay for living in rural isolation," the report says.
"However, Wakatipu and Wanaka are among the fastest growing areas in New Zealand – to the extent that in just 15 years’ time Wakatipu and Wanaka/Central Otago combined will have a resident population as big or bigger than five current DHBs."
It listed South Canterbury, West Coast, Wairapapa, Tairawhiti and Whanganui as those DHBs.
New Zealand doctor Ian Powell, who oversaw the 2011 report's publication, told Crux that this area needs more "clinically-led local empowerment" to ensure that there is more considered planning in the health space.
'Tiles falling out of the ceiling' - West Coast ditches dated hospital
Crux has rounded up a variety of New Zealand healthcare and civic leaders to have a go at answering what a local solution might look like.
Building a new hospital in Queenstown is often the silver bullet solution demanded by the public, and the subject of a Crux petition in 2018, signed by 7,124 residents.
But a new hospital doesn't always lead to happily ever after, Greymouth mayor Tania Gibson tells Crux.
Her district recently went through it; in July 2020 Greymouth opened the doors to Te Nikau Hospital - two years behind schedule and $54 million over budget.

Opened in 2020, Greymouth's new Te Nikau Hospital (Supplied/Te Whatu Ora).
It’s a 50-bed facility, with four critical care beds, surgical services, and secondary maternity services, and three operating theatres.
"I wouldn't say that health outcomes have improved. But I would just say that we are lucky to have a new facility because the other one was so rundown.
"It's maybe still not quite big enough, but that's the thing when we get these new facilities, sometimes they're downsized."
It serves the population of the West Coast - approximately 33,000 people. Comparatively, Lakes Hospital’s 25-bed facility serves 47,000 people, and an annual tourist population that exceeds a million.
But a new hospital can’t fix staff shortages, and at any time they'll be down 50 staff members in the West Coast's health space, Mayor Gibson reports.
It’s a struggle getting nurses and doctors to work on the West Coast, she says, but acknowledges it's a nationwide challenge.

New hospital might not be quite big enough - Greymouth mayor Tania Gibson.
Post-build patients are still frequently choppered to Christchurch for emergencies or have to travel there themselves for specialist appointments.
“For those specialised services we have to go to Christchurch, and it's quite hard on our elderly residents and people struggling with the cost of living.”
Hospital wait times are still long, but it's a "lovely facility" compared to the now demolished building, with its "tiles falling out of the ceiling", she says.
Ageing population - and adventurers
Retired trauma surgeon John Harman has been living in Queenstown for the past few years and told Crux quite frankly it was “concerning” that the area had no trauma care.
Anyone who breaks their legs or has a serious car accident or a heart attack is “a minimum two to three hours away” from high-quality care, Mr Harman says.
There’s a medical term called “the golden hour”, he says.
“If you are more than an hour from an emergency centre, such as an intensive care unit or a trauma centre, your chance of dying goes up by 20 percent.
“In the autobahns in Germany and the ski fields in Switzerland, they have helicopters that are ready to go. They have a trauma centre with a helicopter ready – we don’t have that.”

John Harman and wife Karen Spires says Queenstown Lakes emergency care is 'a very adhoc situation'.
He's also got Queenstown's ageing population and the growing number of retirement villages in the area on his mind - what happens when people have a stroke or a heart attack?
As a 70 year old, it's also a cause of personal concern. His wife, Karen Spires says it is for her too.
There's also the younger adventurers and birthing mothers to think about.
“This is unsatisfactory, and we need to have a solution to fix it”.
He says the current “we’ll just pick them up with a chopper and hope for the best” emergency care model is not good enough.
“No one’s auditing this - the premature deaths, the side effects, the complications. We just know that any other population in New Zealand with 100,000 people is less than an hour’s drive from a major hospital.”
From his experience within New Zealand’s healthcare system, the building of a trauma centre or a public hospital takes at least five to ten years to plan.
And, Queenstown and Central Otago is the fastest growing spot in New Zealand, he points out.
“It’s a very ad-hoc situation with no planning…it’s no use saying, 'oh it’s going to be fixed with a wave of a magic wand', we’ve got to start saying this is a problem.”
New minister responds
New Zealand’s newly appointed health minister Shane Reti has spoken with Crux regarding the state of Queenstown's facilities – and whether they’re adequate for our population.
Upgrades to ageing hospital infrastructure and expansion of existing facilities will be an area of focus for the government, he says.

Minister Shane Reti says upgrades and expansions of facilities will be an area of focus for the new government.
Firstly, he says the new government will reinstate all the beds, operating theatres and radiology services that the previous Government removed from the new Dunedin Hospital, as per their campaign promise.
“When complete, this facility will play a key role in supporting healthcare in the southern region, including Queenstown Lakes and Central Otago.”
This includes 23 inpatient beds, two operating theatres, and a PET scanner for $29.5 million, fully funded as part of the government's programme of capital investment, Minister Reti says.
He agrees many issues impact access to healthcare in rural areas, including Queenstown Lakes and the wider Te Whatu Ora Southern district in this category.
Minister Reti says he is seeking advice from health agencies on how to solve these issues.
“I’m also asking officials for a briefing on all the infrastructure projects on Health New Zealand’s current programme of work, and the health infrastructure deficit.
“I will be working with my colleague, Chris Bishop, in his capacity as Minister of Infrastructure, on any opportunities to improve the speed of delivery of major projects across New Zealand.”
Mr Reti didn't provide any specific remedies for local pain points, and dodged Crux's questions regarding whether the lack of facilities and population size was "concerning".
He also neglected to say whether he found it concerning that the Southland area has the most people waiting for more than two years for elective surgery - 264 people - information that was made public through his parliamentary written question to then health minister Ayesha Verall in August 2023.
The next longest waitlists are in Canterbury, with 113 names, and Taranaki, with 75, while the remaining regions all have fewer than 50.
'If I had the money, I would go private'
So for now, patients like Casey Todd will continue to be asked by visiting outpatient doctors, what the point of her local hospital is, as she sits on waiting lists to receive care.
MRI results have shown that her knee cap has moved inside her leg and is in need of surgery.
"If I had the money, I would go private," she says.
Ms Todd has navigated the difficult southern system with two auto-immune diseases for the past decade, and hospital visits and waiting for them to eventuate make up a large part of her life.
Living in Queenstown is her only option as she is unable to work enough to support herself independently as a result of a Hidradenitis Suppurativa (HS) diagnosis 10 years ago.

She'd go private if she could - Queenstown resident Casey Todd.
HS is a chronic condition that involves lesions developing on the skin, near the armpit, chest and groin, and Ms Todd says they can grow overnight to be as large as a tennis ball.
Twice since her diagnosis, her mum has driven her to Invercargill's A&E to remove painful growing abscesses. On both occasions, Ms Todd received surgery the next day and then stayed in the ICU, whilst her mother stayed in hotels.
The lack of hospital facilities had also split up her family, as without a dementia ward locally her grandmother had to move first to Invercargill, then Cromwell for care, after living in Queenstown her whole life.
Her grandfather would drive through the gorge to Cromwell every Friday before she passed away.
Ms Todd's practised method is to avoid the local Queenstown emergency department unless she’s in desperate need of care, so she’s only visited twice in 2023.
Both times she says she left “with no definitive answers” after spending eight hours at the hospital.
She says it was unclear what was wrong both times.
"I don't blame the staff, they are trying their damnedest, but they just don't have the facilities available to them to do what needs to be done in some cases."
She went to the emergency department for "severe" stomach pain this year, a warning side effect of her new HS injection, but it wasn't clear if it had been caused by the injection.
"You go in there, they give you painkillers after they've assessed you - and then the painkillers jump on top of the pain, and then you're not really feeling the pain anymore."
Since then, she says there's been a few more times where the pain has returned.
"But again, I'm thinking, hopefully, it'll just go away on its own, and it mostly does. I've waited it out, rather than going back for the fourth or fifth time, and just sitting there all day waiting."
During this recent emergency visit, the hospital was unable to perform a required abdominal ultrasound for her stomach pain, so Ms Todd was driven by her mother to the nearby radiology clinic in Frankton with the needle still on her arm for the drip line.
"They only have the little portable machines there. Even though there is a room for an ultrasound machine in the new part of the hospital, there's no machine there, they're still waiting for it. They've been waiting about four years for this machine."
As you've probably noticed, Ms Todd spends a lot of time waiting.
"One of the big problems for me, it has always been and always will be until they fix it, is the Lakes District Hospital...there's no way that that little building can cope with what we have in this district now."